We all know that the immune system plays a vital role as our defense against infections and illnesses. Unfortunately, our immune systems don’t always function properly, and in some cases they can trigger health conditions instead of preventing them. One of these autoimmune conditions is multiple sclerosis, or MS.
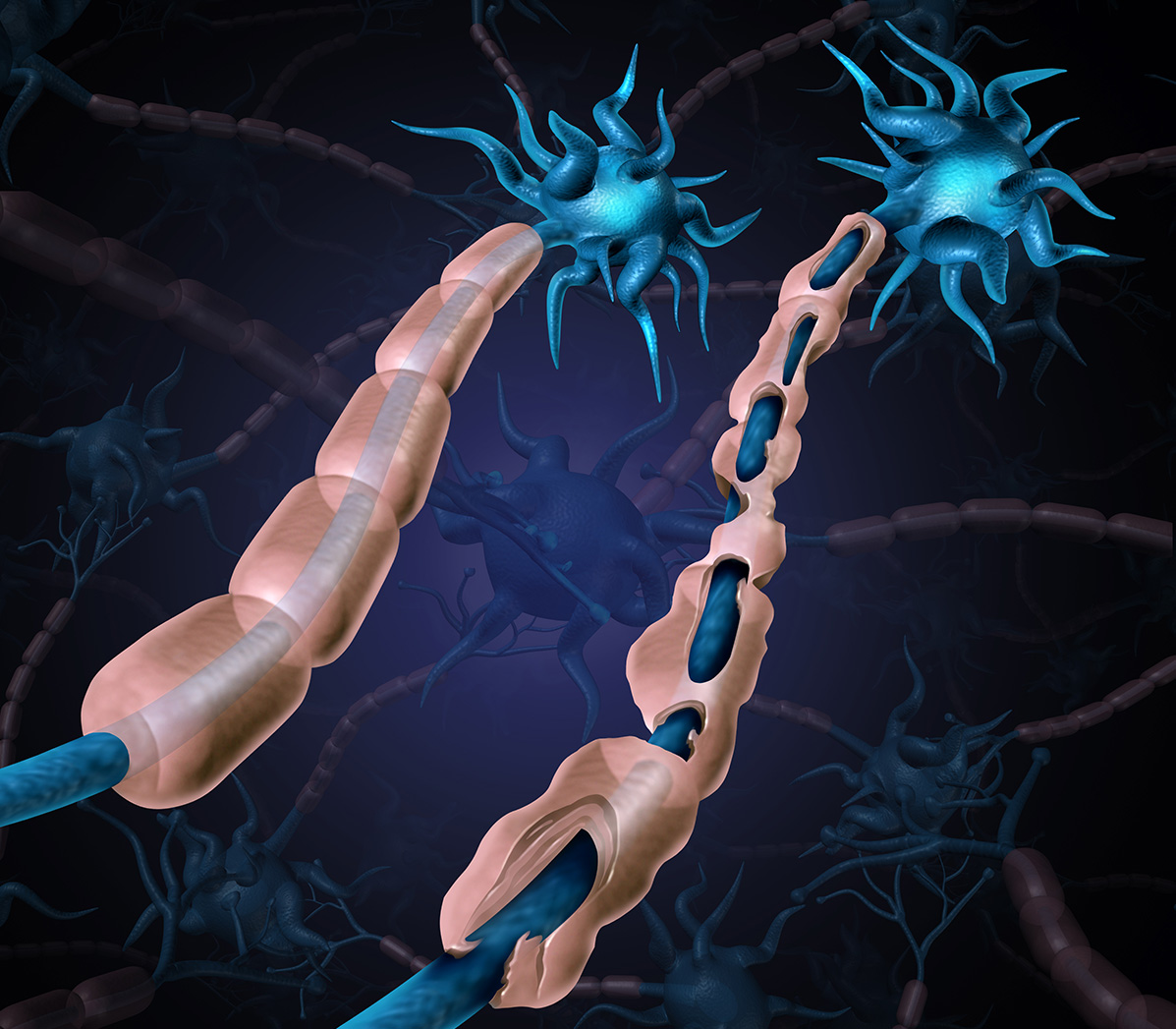
MS is a chronic, incurable disease in which the body’s immune system attacks the central nervous system. The immune system mistakenly targets the myelin sheath, a fatty layer that surrounds and protects nerve fibers. The disease gets its name from the resulting formation of lesions—known as sclerosis—in the damaged areas of the brain, spinal cord and optic nerves.
As the myelin sheath and nerve fibers are damaged or destroyed, electrical signals no longer travel efficiently between the brain and body, leading to a variety of neurological symptoms. The damage caused by MS currently is irreversible, so it’s critical that we recognize the symptoms and take steps to treat them before the disease progresses.
Symptoms and diagnosis
MS is often described as a “snowflake disease” because everyone experiences it in a different way. Some of the most common symptoms include pain, fatigue, numbness or tingling in the limbs, muscle weakness, cognitive changes and vision problems.
Most patients with MS start with a relapse-remitting form of the disease, which is marked by periods of new or worsening symptoms followed by longer periods in which the disease is in a state of inactivity known as remission. A small number of people experience only minor symptoms, but others see a steady worsening of their condition with some transitioning into progressive forms of the disease.
The variability of this disease can make it very difficult to diagnose. There’s no test that definitively proves the onset of MS; instead, a physician typically reaches a diagnosis by ruling out other conditions that result in similar symptoms. Your doctor might recommend an MRI, which can reveal the presence of lesions in the central nervous system, or a lumbar puncture, which can show antibody abnormalities that are indicative of MS.
Getting treatment
If you’re diagnosed with MS, then you’ll need a treatment plan tailored to your unique experience with the disease. The good news is that we’ve seen significant breakthroughs in treatment over the last 20 years, and we now have a number of therapies to manage the symptoms of MS.
Some of the most common treatments for MS are disease-modifying therapies, which suppress the body’s inflammatory response to slow the disease’s progression. For severe relapses, corticosteroids can help reduce inflammation and hasten recovery. To address specific symptoms, a physician might prescribe medications that reduce fatigue, ease muscle stiffness or relieve pain.
A daily regimen of mild to moderate physical activity can also have a positive effect on a patient’s condition by reducing fatigue and improving overall fitness and mood. However, it’s important to avoid overexertion since many people’s symptoms worsen when their body temperature rises.
Living with MS
Nearly 1 million Americans are living with MS, according to the National Multiple Sclerosis Society. The disease typically manifests among younger adults, with the onset of symptoms occurring between the ages of 20 and 40. These patients have long lives ahead of them, and I’m grateful for medical advances that allow them to maintain much of their previous quality of life.
Nonetheless, living with a chronic disease like MS can be difficult, and it’s important to pay attention not only to your physical health but also to your emotional well-being. You should continue to pursue any hobbies or activities that you’re able to perform, and you should seek the help of your friends, family members and physicians when you need support.
While MS might affect your day-to-day life, it doesn’t have to define it.
Robert “Lee” Archer, M.D., is a professor of neurology at the University of Arkansas for Medical Sciences (UAMS) and treats patients at the UAMS Neurology Clinic in the Jackson T. Stephens Spine & Neurosciences Institute.